Steatotic Liver Disease (SLD)

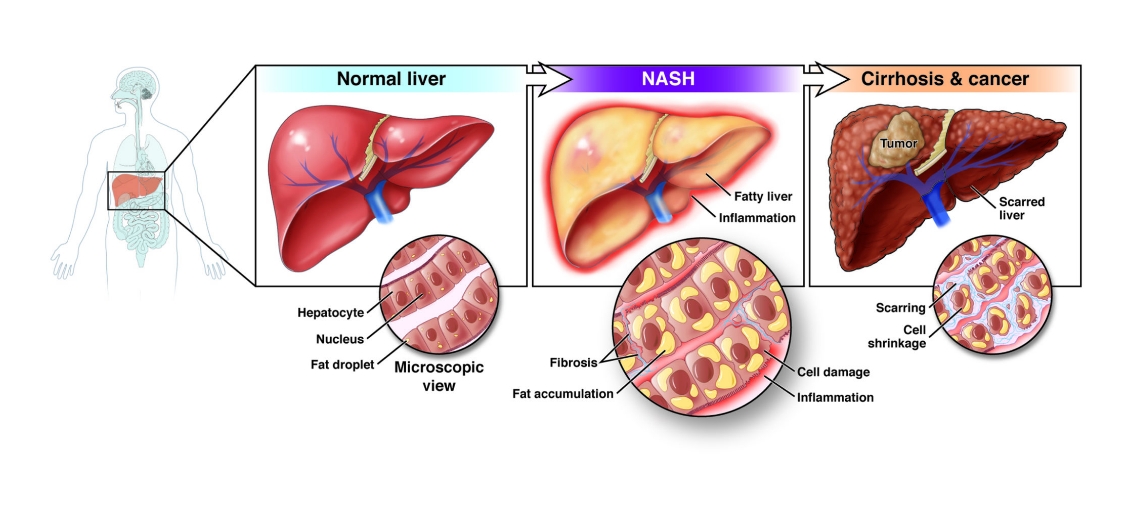
SLD is a medical condition that is characterized by the build up of fat (called fatty infiltration) in the liver.
There are two types of SLD:
Metabolic steatotic liver disease (MSLD), a generally benign condition in which there is fatty infiltration but no inflammation.
Metabolic dysfunction–associated steatohepatitis (MASH), in which there is fatty infiltration along with liver inflammation.
Alcohol use disorder and other conditions can also lead to liver problems. To be diagnosed with either form of SLD, a person must not have a history of heavy alcohol use or another problem that might be causing the liver condition (such as hepatitis C).
Metabolic Steatotic Liver Disease (MSLD)
(MSLD) is a generally benign condition that has become increasingly common as weight gain and obesity have become more common. It is now the most common chronic liver disorder in Australia, United States and other western industrialised countries.
In MSLD, the liver functions normally and there are no symptoms. MSLD is often found when a person has imaging tests of the abdomen for other reasons (such as an ultrasound being done to look for gallstones). If you are overweight, losing weight can reduce the amount of fat in your liver. Aside from this, there is no treatment for MSLD, although you should be vaccinated against hepatitis A and B (which can damage your liver) if you are not already immune.
Many people with MSLD never develop inflammation (MASH), although some do.
Metabolic dysfunction–associated steatohepatitis (MASH)
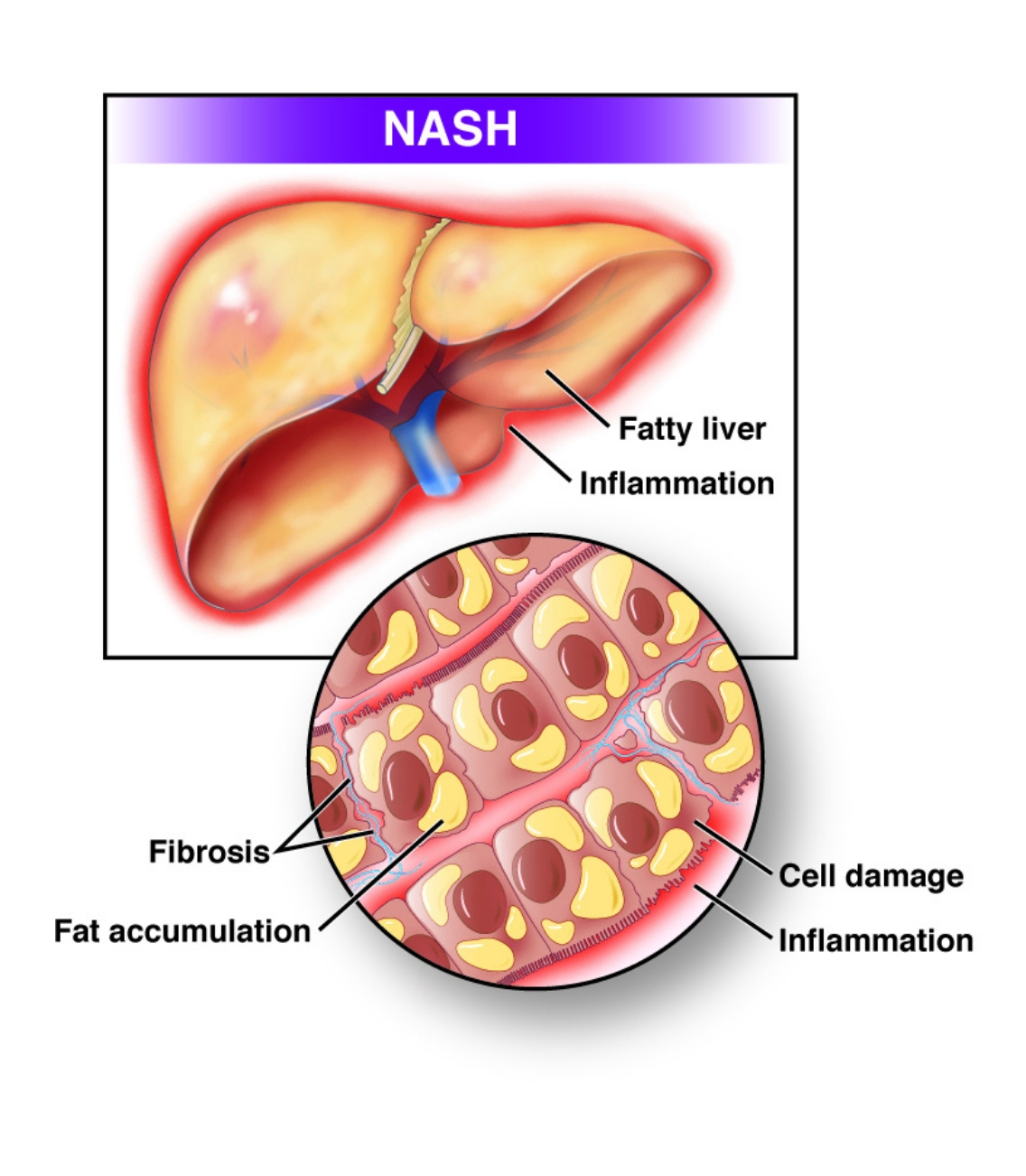
Metabolic dysfunction–associated steatohepatitis (MASH) is a condition that causes inflammation and accumulation of fat and scar tissue in the liver. Although a similar condition can occur in people who have alcohol use disorder, MASH occurs in those who drink little to no alcohol. The exact cause of MASH is unknown. However, it is seen more frequently in people with certain medical conditions such as diabetes, obesity, and insulin resistance. This combination of disorders if often called “metabolic syndrome.”
It is not clear how many people have MASH because it causes no symptoms. However, MASH is diagnosed in about 3 to 5 percent of people in the United States who have a liver biopsy (which may be done to check for a number of different liver conditions). Most people are between the ages of 40 and 60 years, although the condition can also occur in children over the age of 10 years. MASH is seen more often in females than in males.
Treatment of MASH focuses on controlling some of the medical conditions associated with it (such as diabetes and obesity) and monitoring for progression. Some studies suggest that people who drink coffee have a lower risk of developing liver scarring, and some researchers have suggested that moderate coffee consumption may be beneficial. As with MSLD, people with MASH should be vaccinated against hepatitis A and B if they are not already immune.
Associated conditions
Although the cause of MASH is unknown, it is most frequently seen in people with one of more of the following conditions:
- Obesity – More than 70 percent of people with MASH have obesity.
- Diabetes – Up to 75 percent of people with MASH have type 2 diabetes. This is a disorder that disrupts the way your body uses sugar. Normally, sugar gets into the cells with the help of a hormone called insulin, which is made in the pancreas. In people with type 2 diabetes, the body stops responding to normal or high levels of insulin, which causes sugar to build up in the blood; eventually, the pancreas becomes unable to produce enough insulin.
- Hyperlipidemia – About 20 to 80 percent of people with MASH have hyperlipidemia (high blood triglyceride levels and/or high blood cholesterol levels).
- Insulin resistance – Insulin resistance refers to a state in which the body does not respond adequately to insulin, but the person does not yet have type 2 diabetes. This often occurs in people with hyperlipidemia who have obesity; this group of symptoms is known as the metabolic syndrome and is frequently seen in people with MASH.
- Drugs and toxins – Several drugs used to treat other medical conditions have been linked to MASH, including Amiodarone, Tamoxifen, perhexiline maleate, Steroids and synthetic estrogens. Certain pesticides have also been linked to MASH.

Call us today for an appointment at Gledswood Hills or Shellharbour
Symptoms
Most people with MASH have no symptoms. Rarely, MASH is found (after testing) in people with fatigue, a general feeling of being unwell, and a vague discomfort in their upper right abdomen, although it is not clear if these symptoms are related to MASH.
Diagnosis
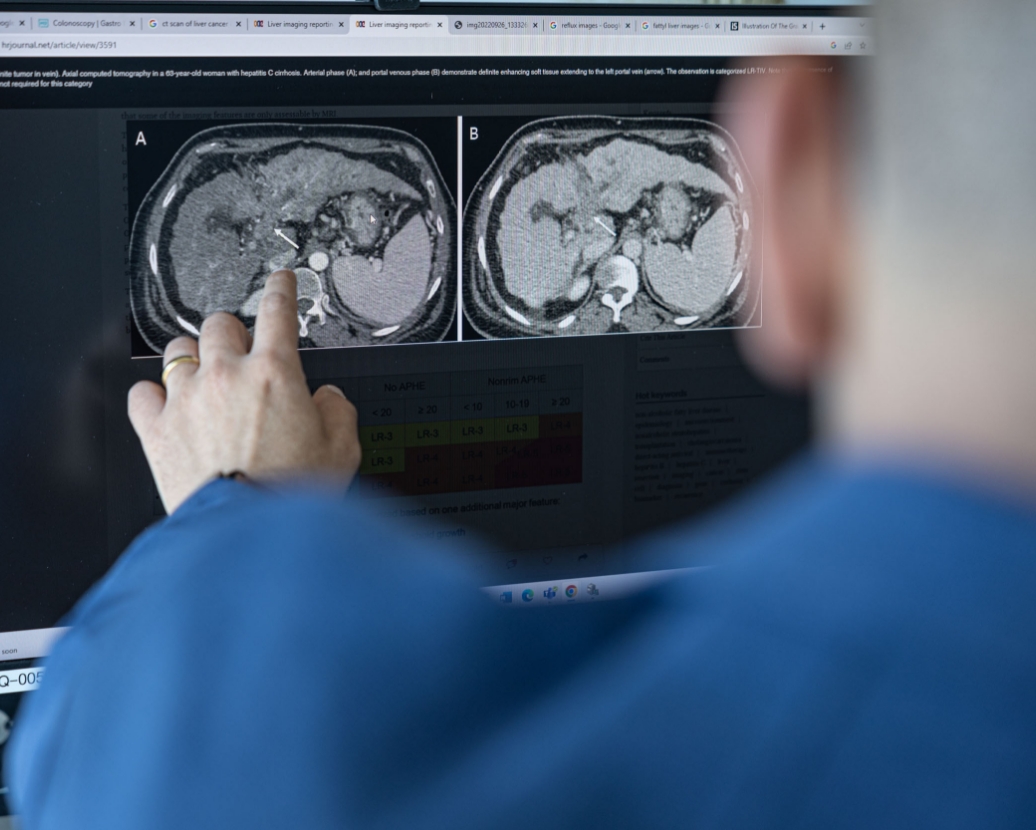
MASH is most often discovered following routine blood tests. Additional tests help confirm the presence of MASH and rule out other types of liver disease. Imaging tests (such as ultrasound, CT scan, or magnetic resonance imaging [MRI]) may reveal fat accumulation in the liver but cannot differentiate MASH from other causes of liver disease that have a similar appearance.
A liver biopsy may be required to confirm MASH if other causes of liver disease cannot be excluded.

Blood tests to measure liver function measure levels of substances produced or metabolized by the liver. These levels can help to diagnose MASH and differentiate MASH from MSLD. Levels of two liver enzymes, aspartate aminotransferase (AST) and alanine aminotransferase (ALT) are elevated in about 90 percent of people with MASH.
Additional blood tests are useful for ruling out other causes of liver disease. These usually include tests for viral hepatitis (hepatitis A, B, or C), and may include tests for less common causes of liver disease.
Although other tests may suggest a diagnosis of MASH, sometimes a liver biopsy is required to confirm it. A liver biopsy may be needed if other causes of liver disease cannot be ruled out with standard blood and imaging tests. A liver biopsy can also help determine the severity of inflammation, detect liver scarring (called “fibrosis” or, in severe cases, “cirrhosis”), and may provide clues about the future course of the condition. The procedure involves collecting a small sample of liver tissue, which is sent to a laboratory for microscopic examination and biochemical testing. More detailed information about liver biopsies is available in a separate topic review.
FibroScan is a noninvasive test that uses ultrasound to determine how “stiff” the liver is. This stiffness can then be used to estimate how much scarring there is in the liver and to determine if cirrhosis has developed. Where available, FibroScan is an alternative to liver biopsy for detecting liver scarring.
Treatment
There is no cure for MASH. Treatment aims to control the conditions that are associated with MASH such as obesity, diabetes, and hyperlipidemia. Several experimental treatments are being studied with drugs that treat insulin resistance.
Losing weight can help to reduce levels of liver enzymes and insulin and can improve quality of life. Weight loss should be gradual since rapid weight loss has been associated with worsening of liver disease. Your GP or nutritionist can provide an individualised weight loss plan.
People with MASH, early cirrhosis, and obesity who undergo bariatric (weight loss) surgery often have improvement of their liver disorder.
For people with severe forms of MASH who do not also have diabetes or heart disease, doctors sometimes recommend supplements of Vitamin E. There is some evidence that vitamin E might reduce some of the liver damage that occurs as part of MASH, but the evidence is weak, and there is also evidence that high-doses of vitamin E supplements increase the risk of death. Do not take vitamin E unless your doctor recommends it.
People with MASH should avoid drinking alcohol, because it can worsen liver disease.
Prognosis
However, in some people, MASH gets worse over time. The most serious complication of MASH is cirrhosis, which is when the liver becomes severely scarred. Cirrhosis does not always cause symptoms, but when symptoms do occur, they can include swelling in the legs, trouble breathing, or fatigue. Older people with diabetes may be at increased risk for developing cirrhosis.
People with MASH often have metabolic syndrome (insulin resistance, obesity, and hyperlipidemia). Metabolic syndrome puts you at increased risk for heart disease. The good news is that the treatments for MASH (particularly weight loss) also help treat the other problems that are part of the metabolic syndrome.
MASH is typically a chronic, life-long condition. It is difficult to predict the progression of MASH in an individual. Few factors have been useful in predicting the course of this condition, although features in the liver biopsy can be helpful.
The good news is many people with MASH will not develop serious liver problems. One study showed that most people with MASH live as long as those without it. Furthermore, liver function tests are stable over time in most people with MASH.

